It’s important to get an annual dental exam; important to get your teeth cleaned but also important to check on the status of the teeth and gums. But did you also know that it’s important to get a routine periodontal examination? The American Academy of Periodontology believes that all adults should receive a regular yearly periodontal exam.
What is a Comprehensive Periodontal Exam?
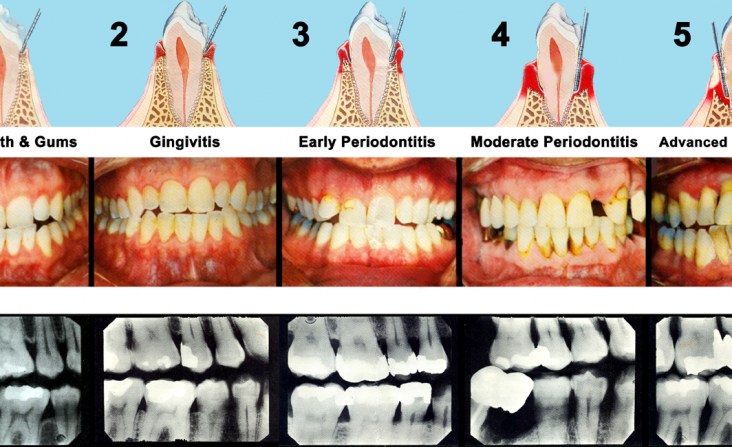
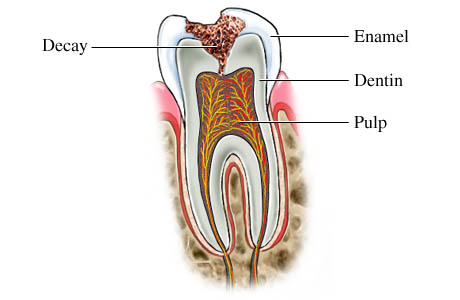
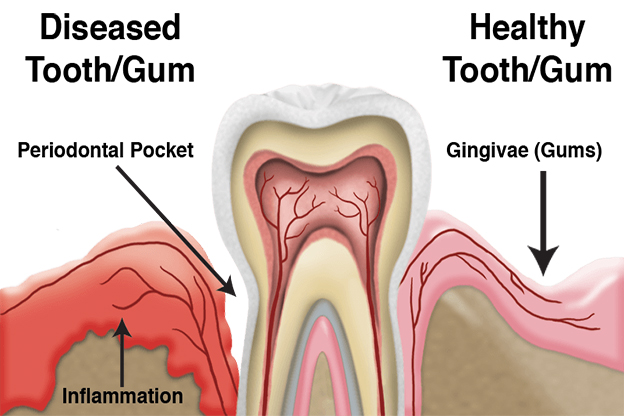
A Comprehensive Periodontal Exam (CPE) assesses your periodontal health by examining the teeth, plaque, gums, bite, bone structure, any risk factors—life factors as well as possible genetic factors—for evidence or potential indications of impending Periodontal disease. During a CPE, Dr. Manhart will assess your periodontal health in relation to these factors. Periodontal disease is prevalent in the United States, and unfortunately most people don’t realize that they have the disease. Consider the CPE to be an evaluation of the health of the entire mouth. No, you may not have periodontal disease—and hopefully you never get periodontal disease—but finding periodontal disease early is the key to a quick and successful treatment.
The Link of Periodontal Disease to Other Systemic Disease
There is evidence that some types of systemic disease are linked to periodontal diseases. No, this does not mean that if you have periodontal disease you will contract diabetes or heart disease, but it’s possible that the periodontal disease could be a trigger for other disease, especially since some types of systemic diseases such as cardiovascular disease, heart disease, and diabetes are known to be linked to inflammation within the body.
You can also do a number of things at home to help prevent periodontal disease (remember, however, that periodontal disease is linked to certain genetic factors, and it’s possible to contract the disease even with the best oral care regimen). Make sure that you’re brushing your teeth twice daily, for two minutes, and that you’re brushing all the brushable parts within your mouth such as the teeth, gums, and tongue (remember the tongue is home to lots and lots of bacteria!). Make sure to floss once daily, cleaning the teeth all the way to the gum line. And pay attention to the life factors that can contribute to periodontal disease, and remember to pay a regular visit to your periodontist, Dr. Manhart, at least once every year for a CPE.